Diabetic Retinopathy
What is diabetic retinopathy?
Diabetic retinopathy is a health issue that can result from having diabetes, where this disorder affects the eye by damaging the blood vessels in the retina, the light-sensitive layer at the back of the eye. In its early stages, diabetic retinopathy may not cause any signs, or may only lead to minor visual problems. However, in advanced cases, it can lead to complete vision loss. This condition can occur in individuals with either type 1 or type 2 diabetes. The likelihood of developing it increases with the duration of diabetes and poor control of blood glucose levels.

You may not experience any warning signs of retinal problems due to diabetes. But over time and with the progression of the disease, a range of symptoms such as seeing black spots or strings floating in your vision, known as floaters, blurry vision that comes and goes, frequent changes in vision clarity, the appearance of dark or empty areas in your vision, and gradual loss of vision might occur.
To maintain your eye health and reduce the risk of vision loss, it is very important to manage your blood sugar levels effectively. If you have diabetes, an annual eye exam with pupil dilation is crucial, even if your vision seems fine.
For women, diabetes that develops during or before pregnancy can increase the risk of diabetic retinopathy. Therefore, if you are pregnant, it is essential to follow the ophthalmologist’s recommendations regarding additional eye examinations during pregnancy.
In case of any sudden changes in vision, whether it be blurriness, spots, or distortion, it is imperative to contact an ophthalmologist as soon as possible.
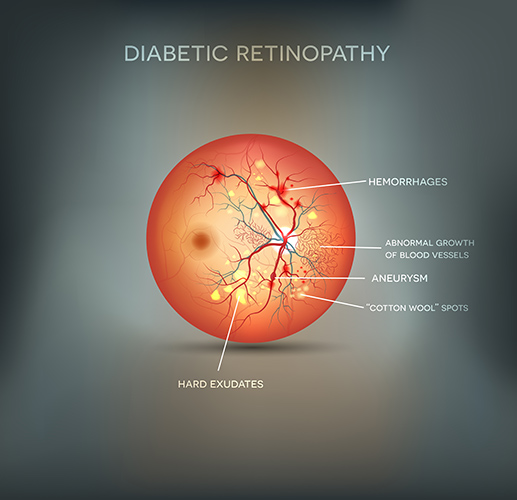
Over time, high blood sugar levels can lead to the blockage of the small blood vessels that nourish the retina, cutting off its blood supply. In response, the eye attempts to grow new blood vessels, but these vessels are often abnormal and leak easily.
There are two types of diabetic retinopathy:
Early diabetic retinopathy: Also known as non-proliferative diabetic retinopathy (NPDR), this is the more common type where new blood vessels aren’t being formed.
In NPDR, the walls of the blood vessels in the retina weaken, leading to the protrusion of small bulges that may leak blood and fluids into the retina. Larger vessels may dilate and become irregular in diameter. NPDR can progress from mild to severe as more blood vessels become blocked.
Advanced diabetic retinopathy: Diabetic retinopathy can advance to this more severe stage, known as proliferative diabetic retinopathy (PDR). In this stage, damaged blood vessels are closed off, leading to the growth of new, abnormal blood vessels in the retina. These new vessels are fragile and prone to leaking into the vitreous, the clear fluid that fills the middle of the eye.
Eventually, the scar tissue caused by the growth of new blood vessels can lead to the retina detaching from the back of the eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure may build up in the eyeball, potentially damaging the optic nerve that transmits images from the eye to the brain, resulting in glaucoma.
It is crucial to monitor and manage these conditions carefully to prevent further damage to the eye.
Anyone with diabetes can face diabetic retinopathy. The risk of this eye disease increases due to various factors including:
Having diabetes for a long time.
Poor control of blood sugar levels.
High blood pressure.
High cholesterol levels.
Pregnancy.
Smoking.
Complications of diabetic retinopathy
Diabetic retinopathy causes the formation of abnormal blood vessels in the retina, which can lead to complications that significantly affect vision, including:
Bleeding into the vitreous. The newly formed blood vessels may leak blood into the clear, gel-like substance that fills the eye. If the bleeding is minor, you might see a few dark spots in your vision. However, if there is significant bleeding, the vitreous can fill with blood, completely blocking vision.
Vitreous hemorrhage typically doesn’t cause permanent vision loss and the blood may clear from the eye within a few weeks or months. Vision may return to normal unless the retina is damaged.
Retinal detachment. The growth of abnormal blood vessels and the accompanying scar tissue can cause the retina to detach from its normal position at the back of the eye, leading to potentially total vision loss.
Glaucoma. The new blood vessels growing in the front part of the eye can interfere with the normal flow of fluids, increasing eye pressure, which can damage the optic nerve responsible for transmitting images from the eye to the brain.
Blindness. If diabetic retinopathy, macular edema, and glaucoma are not managed, they can lead to total vision loss.
Prevention of diabetic retinopathy
While it’s not always possible to completely prevent diabetic retinopathy, regular eye exams, efficient management of blood sugar and blood pressure levels, and early intervention for any vision problems can help prevent severe vision loss.
To reduce the risk of diabetic retinopathy if you have diabetes, it’s advisable to follow these guidelines:
- Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Aim for about 150 minutes a week of moderate aerobic activity, such as walking. Follow your doctor’s instructions for diabetes medications, whether they’re taken by mouth or insulin.
- Monitor your blood sugar level. You might need to check and record your blood sugar levels several times a day or more frequently if you’re ill or under stress. Ask your doctor how often you need to test your blood sugar.
- Ask your doctor about a glycosylated hemoglobin test. This test reflects your average blood sugar level for the two to three months before the test. For most people with diabetes, the American Diabetes Association recommends an A1C level below 7%.
- Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly, and losing excess weight can help. You might also need medication.
If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases the risk of diabetes complications, including diabetic retinopathy.
Pay attention to vision changes. Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty, or hazy.
Remember, having diabetes doesn’t necessarily mean you’ll lose your sight. Effectively managing diabetes can help prevent complications.
Working Hours
Saturday
7 pm to 9 pm
Sunday
7 pm to 9 pm
Monday
7 pm to 9 pm
Tuesday
7 pm to 9 pm
Wednesday
7 pm to 9 pm
Thursday
Closed
Friday
Closed
Ramadan Working Hours
Saturday to Wednesday from 9 pm to 11 pm
Location
21st Ismail Ramzy st. – El-Bostan – Heliopolis – 4th floor
01110114354
01222422637
0226331026
(7 pm to 9 pm)
Make Appointment
Always happy to receive your inquiries
