Keratoconus
Corneal Characteristics and Functions
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. It plays a crucial role in the eye’s optical system by focusing incoming light onto the retina. Its main function is the refraction or bending of light, which contributes to clear vision.
The cornea is unique among body tissues as it contains no blood vessels; it receives oxygen directly from the air. This aspect helps maintain its transparency, which is essential for its optical function. The cornea has a complex structure composed of several layers: the epithelial layer (the outer layer acting as a protective barrier), the basement membrane, the stroma (the actual cornea), and the endothelium (the inner layer).
Functionally, the cornea is responsible for approximately 70% of the eye’s focusing power. Its transparency and refractive strength are crucial for effectively directing light towards the lens, which then fine-tunes the focus. Maintaining corneal health is vital for preserving good vision. Any changes in its shape or transparency, as seen in conditions such as keratoconus, can lead to blurred vision and other visual problems.

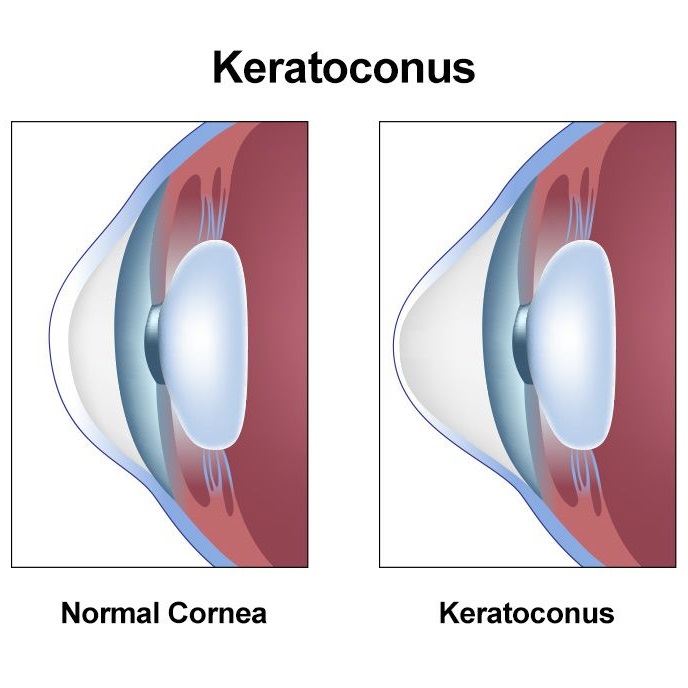
Keratoconus is a degenerative eye condition where the cornea becomes thin and starts to bulge outward, forming a cone shape instead of its normal round shape. This alteration in shape causes vision distortion because it interferes with how light rays pass through the eye, leading to astigmatism and nearsightedness.
Keratoconus is a progressive condition, meaning it worsens over time, especially if left untreated. It typically begins in adolescence or early twenties and gradually progresses over several years. The exact cause of this condition is not fully understood, but genetic factors are believed to play a significant role in its development.
Early treatment is crucial for controlling the progression of vision deterioration and reducing the need for complex surgical interventions in the future. Treatment options include the use of specialized contact lenses, ultraviolet light treatment (corneal collagen cross-linking), and the implantation of intracorneal rings. In advanced cases, corneal transplantation may be necessary
Keratoconus is generally not considered dangerous, but it significantly affects vision quality and may require advanced medical interventions if not properly managed. In the early stages, the effects are limited and may include blurred vision and increased sensitivity to light. As the disease progresses, vision distortion may increase, making it difficult for those affected to perform their daily activities normally.
In very advanced cases, keratoconus may lead to severe thinning of the cornea, increasing the risk of corneal rupture or perforation, a condition requiring emergency surgical intervention. However, this is rare and can be avoided in most cases through regular monitoring and early treatment.
Effective treatment and regular follow-ups with an ophthalmologist play a crucial role in controlling the disease and minimizing its impact on the quality of life. With medical technology advancements, there are now effective treatment options available that help control the disease’s progression and improve vision.
The exact cause of keratoconus is unknown, but research suggests a role for genetic and environmental factors. Studies have found a genetic predisposition to keratoconus, often recurring within specific families.
In addition to genetic factors, environmental factors are believed to contribute to the condition’s development. One such factor is excessive eye rubbing, which can lead to corneal thinning and shape alteration. Individuals with severe allergies, especially eye allergies, may be more prone to frequently rubbing their eyes, increasing the risk of developing keratoconus.
Some medical conditions are also associated with an increased risk of keratoconus, such as Down syndrome and systemic diseases like rheumatic fever. However, the primary cause of keratoconus remains unclear, believed to result from a complex interaction between genetic and environmental factors.
Symptoms of Keratoconus
Keratoconus presents a variety of symptoms, which vary in severity depending on the stage of the condition. In the early stages, patients might not notice any clear symptoms, but as the disease progresses, symptoms may include:
- Blurred vision: The most common symptom, resulting from the change in the shape of the cornea.
- Changes in the prescription of glasses or contact lenses: Patients might need to change their prescription frequently.
- Sensitivity to light and glare: Patients may struggle with bright light.
- Seeing halos around lights: Particularly at night, patients may notice halos around light sources.
- Difficulty with night vision: Deterioration of vision in low light.
- Astigmatism: Distorted vision due to the change in the shape of the cornea.
- Eye strain: Patients may experience eye fatigue after prolonged periods of visual activity.
It’s important to note that symptoms can change and worsen as the disease progresses. Therefore, regular eye examinations and early diagnosis play a vital role in effectively managing keratoconus.
Prevention of Keratoconus
Keratoconus is a degenerative condition that affects the cornea, causing it to change shape into a cone, which impacts vision. It cannot be fully prevented due to possible genetic factors. However, the risk of exacerbation can be reduced by avoiding continuous eye rubbing, as repeated pressure can contribute to altering the shape of the cornea. Regular eye health monitoring is advised to detect any changes early.
Vision Improvement Post-Keratoconus Surgery
The improvement in vision after keratoconus surgery depends on the type of surgery used and the condition of the eye. Typically, patients begin to notice improvement within weeks to months after the surgery. In some cases, patients may require glasses or contact lenses post-surgery to achieve the best possible vision. Following medical care after surgery and adhering to the doctor’s instructions is crucial.
Risks of Not Undergoing Keratoconus Surgery
If keratoconus is left untreated, the condition can worsen, leading to deteriorating vision. In advanced stages, it may become difficult to correct vision with glasses or contact lenses. In severe cases, a corneal transplant may be necessary to restore vision. Therefore, consulting with an ophthalmologist to determine the best treatment options is advised.
Treatment of Keratoconus
The treatment of keratoconus involves using glasses or rigid contact lenses to correct vision. In more advanced cases, doctors may recommend surgical procedures such as corneal strengthening with ultraviolet rays or implantation of intracorneal rings. In rare cases, corneal transplantation may be necessary.
Diagnosis of Keratoconus
Keratoconus is typically diagnosed through a detailed eye examination using techniques such as corneal tomography, which provides an accurate picture of the cornea’s shape. Doctors may also use other tests such as corneal thickness measurement and vision tests to confirm the diagnosis.
Advantages of Contact Lenses Over Glasses
Contact lenses offer a wider field of vision and are not affected by weather conditions like rain or sweat. They are also better for physical and sports activities. Specifically, rigid contact lenses provide clearer vision for keratoconus patients than glasses.
Corneal Cross-Linking Procedure Steps
The corneal cross-linking procedure, also known as ultraviolet corneal strengthening (CXL), involves applying vitamin B2 (riboflavin) to the cornea and then exposing it to ultraviolet light. This process strengthens the corneal collagen fibers and stops or slows the progression of the condition.
Complications of Keratoconus Treatment Procedure
Like any surgical procedure, keratoconus treatment involves some risks, such as infection, corneal inflammation, changes in vision, or in rare cases, loss of vision. However, when performed by a qualified specialist, these risks are relatively low.
Working Hours
Saturday
7 pm to 9 pm
Sunday
7 pm to 9 pm
Monday
7 pm to 9 pm
Tuesday
7 pm to 9 pm
Wednesday
7 pm to 9 pm
Thursday
Closed
Friday
Closed
Ramadan Working Hours
Saturday to Wednesday from 9 pm to 11 pm
Location
21st Ismail Ramzy st. – El-Bostan – Heliopolis – 4th floor
01110114354
01222422637
0226331026
(7 pm to 9 pm)
Make Appointment
Always happy to receive your inquiries
